This is how our application simplifies the booking and administration process. Interested >>
Filling the intervertebral disc spaces - Percutaneous cement discoplasty (PCD)
The spine consists of vertebrae and intervertebral discs. Intervertebral disc degeneration may be accompanied by pain, posture changes, and additional symptoms. Filling up the flattened intervertebral disc spaces may provide a solution if surgical treatment is necessary.
What does intervertebral disc loss with instability mean?
One or more of the cartilagenous structures, the intervertebral discs, which hold the vertebral bodies together in a flexible, but tight manner, lost their contents (in everyday language: they are worn down), because of which the originally tight connection between the vertebral bodies has become inflexible, and instable. Symptoms mainly present as pain which increases on loading at the affected spinal segments, radiating to the lumbar spine, in the aspect of the pelvis transversally, maybe in the buttocks, or on the back surface of the thighs. Rarely, temporary numbness may present too.
The degeneration or wear down of the intervertebral discs affect almost everyone, and it is more common with advanced age. Surgical treatment is not necessary if the degeneration of the intervertebral discs is not accompanied by instability, it does not cause significant deformities, and the consequent “calcification” does not narrow the spinal canal. This surgical information leaflet concerns those cases, where the pain, which increases on loading is caused by the content loss of one or more thoracic or lumbar intervertebral discs, the patient’s load capacity has decreased significantly, and they look for support in standing and walking.
Which are the potential symptoms of a degenerated intervertebral disc with instability?
- Intensive local pain, which decreases in lying, and increases on load.
- Postural disorder (slouching forward), which stops in lying.
- The symptoms decrease when the patient leans on something, or uses a wheeled aid (rollators, shopping cart).
- Depression, sleep disturbances, loss of appetite.
- Percutaneous cement discoplasty cannot be performed on its own if lower limb symptoms are also present: pain, numbness, clumsiness or weakness of the limbs, symptoms similar to radiation around the chest or the abdomen.
How is a degenerated intervertebral disc with instability diagnosed?
- Conventional X ray scan (in standing). This is the most suitable imaging study to comprehensively evaluate the spine, and to analyze the statical and morphological changes. In order to detect instability, images are also taken of the affected spinal segments in a loaded position and in lying. Thorough analysis of the posture may require the computerized stitching of the images, or that a full body X ray scan (EOS) is taken.
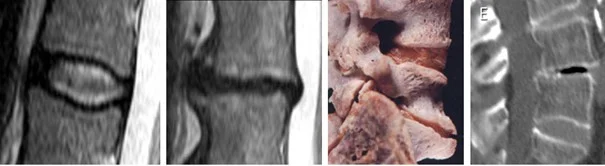
- Magnetic resonance imaging (MRI) based on which mainly the bony involvement of the spine, and any significant narrowing of the spinal canal are ruled out, which may be contraindications.
- Computerized tomography (CT) based on which the operable intervertebral disc spaces are eventually identified, and the surgery could be planned.
What are the treatment options?
Basically, there are two types of treatment options available:
Non surgical (conservative) treatment:
Conservative treatment is used in all cases, when despite the intervertebral disc degeneration, the patient’s quality of life is acceptable to them, their ability to walk and their load capacity are maintained, or the pain can be well controlled by drugs, and physical therapy treatments, the spine is not significantly deformed, and the stability of the spine can be restored by physiotherapy.
The aims of conservative treatment:
- Reducing pain.
- Restoring the stability of the spine, creating the muscle brace.
- Preventing spinal deformation.
Conservative treatment methods:
- Decreasing the load until pain tolerance.
- Pharmacological treatment (even anti inflammatory drugs administered in infusion), and other physical therapy, and alternative methods.
- A soft back brace may be helpful in the painful period or when a larger load is expected (in case of shopping or cleaning), but it makes the core stabilization musculature weaker, so wearing it constantly is disadvantageous.
- The patient may get a so called active back brace that consists of metal support, which is adjusted to the spine that was straightened as possible, a belt with a hook and loop fastener, which constricts the pelvis, and straps, which pull the shoulders to the metal plate that is adjusted to the spine.
In the long term:
- Changing the lifestyle: reducing (eliminating) alcohol consumption, and smoking, changing the eating habits, reducing the overweight, preventing stress, etc.
- Elimination of sleep disturbances, treatment of associated psychosomatic diseases (as early treatment and cure as possible for e.g., chronic gynecological, cardiovascular diseases).
- Restoring the mental resilience and mood.
- Increasing activity: performing regular physiotherapy (individual education), and gait exercises.
- Complex rehabilitation treatments used from time to time may help in the maintenance of the condition.
Surgery may become necessary if improvement is not detected in terms of the pain, and the load capacity of the spine does not increase despite the non surgical treatment with adequate quality and duration.
Surgical treatment:
The aims of the surgical intervention:
- To increase the height of the empty and instable intervertebral disc space, and to permanently maintain the achieved space height, which results in immediate pain relief.
- To decrease any potential newly developed spinal deformities as possible.
Filling the intervertebral disc spaces through the skin (percutaneously) cannot be performed in the following cases:
- If the act of filling has technical (local) contraindications: e.g., the intervertebral disc is not empty enough, or it has already become rigid. There is no point in performing this surgery in cases like this.
- An explorative, open corrective surgery may be performed if a great structural deformity is detected, which cannot be corrected in lying.
- If there is a too large narrowing of the spinal canal, and there is a risk that this surgery may aggravate it.
- If the patient is unfit for anesthesia or surgery e.g., having poor general condition, hemophilia, or anemia, etc.
- If the patient has the above mentioned signs and symptoms, which are not associated with the vertical instability. Signs of neurological compression, or the narrowing of the spinal canal is present. An open technique should be used in these cases, if possible.
What happens in the operating room?
The empty and flat intervertebral disc spaces are filled up through the skin (percutaneously) from a tube with a diameter of about 5 mm, which ends in a cone. A device is inserted into the area of all intervertebral disc spaces (from the right or the left side depending on the direction from where the asymmetrical degenerated space should be corrected). During the initiation of the operating channel and the duration of the whole surgery, the precision of the working process is controlled from two directions by using an X ray image intensifier.

A semifluid, viscous filling material (bone cement or PMMA i.e., poly methyl methacrylate) is injected into the prepared intervertebral disc space. The material fills out the empty space, which is bordered by the bony endplates from the direction of the head and the legs, and the degenerated and thinned intervertebral disc wall centrally. We wait until the cement hardens (10 14 minutes), then the injecting device is removed. Usually, the wound, which is only a few millimeters big, is not stitched up, only glued.
This procedure may be repeated by every one or two intervertebral discs, until the intervertebral discs which are marked for surgery are treated. A bidirectional follow-up X ray scan is performed at the end of the surgery.
What happens if the justified surgical treatment is not performed?
- The condition may lead to chronic pain syndrome, it could occur that the spine can be loaded for continually shorter periods of time with more and more pain, or that loading is not possible.
- The quality of life may deteriorate further.
- A surgery performed later may become more difficult technically, and its effectiveness may decrease.
If you have any questions, please send a letter to magankorhaz@bhc.hu!
