This is how our application simplifies the booking and administration process. Interested >>
Revision total hip replacement surgery
If the results of physical examinations, X-ray scans or other imaging studies justify it, medical specialists may recommend the replacement of a previously implanted prosthesis for the purpose of alleviating the complaints.
The problem may be indicated by pain, which may increase on load or when walking for a longer period of time, it could decrease or cease at rest, or it could radiate to the groin at the front, to the thighs or knees.
Additionally, a few of the frequent issues are decreasing walking ability and walking distance, limping, and limb shortening, along with the development of a walking disability in case of a fracture or a dislocation.
Skin redness, swelling, fever, and chills may be detected if infection develops.
When might it become necessary to perform a revision total hip replacement surgery?
One of the joints which are exposed to the most load is the hip joint; therefore, loosening is the most common long-term reason for a prosthesis replacement.
A revision total hip replacement surgery is justified in the following cases:
- mechanical loosening can be detected in any of the components,
- joint infection,
- the implanted prosthesis had become instable,
- the products of wear down induced an inflammatory process,
- the bone split or fractured around the prosthesis,
- the prosthesis is worn down or broken.
How is the replacement of the prosthesis performed?
The surgery is performed in spinal or general anesthesia (narcosis). The joint is explored by using or excising the old incision – rarely, a new incision is used. The incision is always made in a way, so that the surgeon can have the best access to the joint. The replacement of the prosthesis usually requires a greater incision and may be accompanied by greater blood loss than the original intervention.
The hip joint can be accessed from multiple directions from the front, the side, or from the back too. When selecting the incision type, it is not the esthetic aspects which are prioritized, the goal is to lessen the burden of the soft tissues, the circulation, and the thinned bone structure.
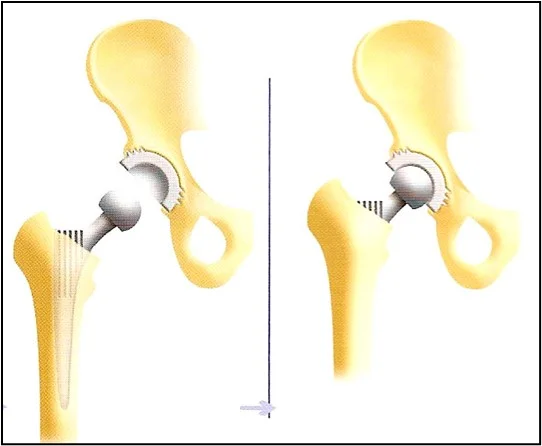
Surgical bleeding reduction is performed once the tissues underneath the skin had been opened. Afterwards, we will reach the joint and the prosthesis, making sure that the musculature remains intact. The original prosthesis will be turned inside out from its socket, and the components are carefully removed.
Tissue, bone and bone marrow biopsies will be taken, which will be sent for laboratory tests for the purpose of detecting the presence of any potential infections.
Following this, the surfaces of the bones and the medullary cavity will be adjusted, and if necessary, it will also be built up with bone, or other components. Then all the components of the new cemented or non-cemented prosthesis will be built up, securing it with screws and/or wires, if needed.
The stem will be placed in the socket with the head after which we will functionally test the prosthesis.
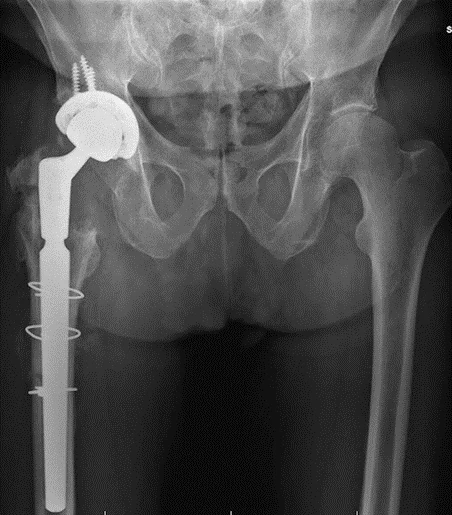
In order to drain the blood that accumulates in the wound, one or two drains will be inserted to the surgical site. The wound is closed, and you will get a sterile cover. A follow-up X-ray scan will be performed at the operating table.
Instruments and implants, which underwent central or individual sterilization and multiple checks are used during the intervention.
It is important to select the time of the surgery, and to thoroughly plan and prepare the intervention. Even with the highest level of care and the most professional approach, rarely it may occur that a new prosthesis cannot be implanted. In that case, a so-called “floating hip” will be created (this is called Girdlestone’s condition).
What happens if your hip prosthesis is not replaced?
Further complications may develop when the prosthesis replacement is delayed. An increase in pain and a decrease in the quality of life can be expected. The level of disability can aggravate further, moreover, an inability to walk may develop. Additionally, the efficiency of a surgery which is performed later may decrease.
If you have any questions, please send a letter to magankorhaz@bhc.hu!


