This is how our application simplifies the booking and administration process. Interested >>
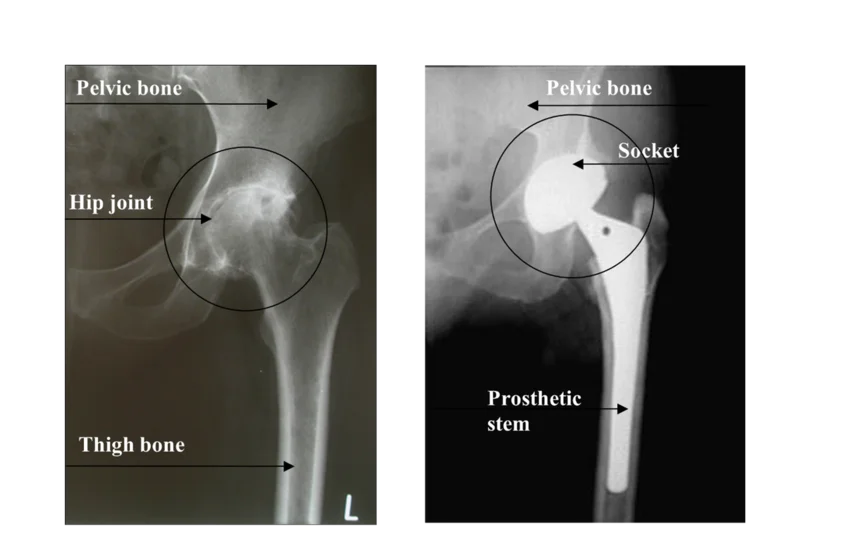
Hip replacement surgery
A hip replacement surgery may be necessary if the symptoms are caused by hip joint wear (hip arthrosis) that is confirmed by physical examination, and X-ray scans.
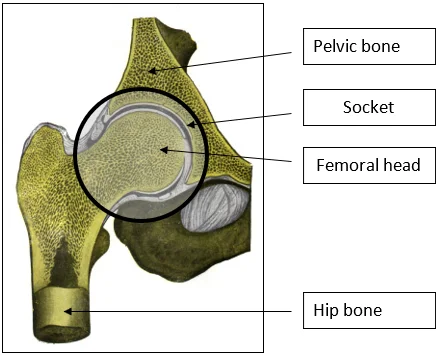
How is the hip joint built?
One of the constituents of the hip is the concave part of semispherical shape covered with cartilage: the socket, which embraces the spherical femoral head also covered with cartilage. The joint is kept in its place by the joint capsule and by strong ligaments, and it is moved by the muscles inserted on the two bones forming the joint.
What happens in case of joint wear (arthrosis)?
- The coverage of hyalin cartilage in the joint wears out and becomes uneven.
- Friction increases during movement.
- The inner membrane of the joint capsule becomes inflamed upon the effect of the detaching cartilage pieces.
- The production of joint fluid is increased which leads to tightness.
- The developing calcification results in the reduction of the joint’s range of motion and the movement becomes painful.
What causes joint wear?
Primary joint wear (primary arthrosis).
In this case, even the most thorough examinations cannot find out what caused the cartilage wear of the hip. Biological aging and degenerative changes may play a great role in the development of the disease
Secondary joint wear (secondary arthrosis).
In this case, previous diseases cause cartilage destruction.
- In childhood:
- Congenital hip dysplasia
- Perthes disease: the second most common hip disease which occurs between the ages of 3 to 13 years. It is associated with the dysfunction of the blood circulation in the femoral head.
- In adolescence:
- Misalignment of the femoral head in the line of growth: a disease based on traumatic or hormonal dysfunction.
- Joint injuries, inflammations.
- In adulthood:
- Fractures of the femoral neck and in the region of the.
- Joint inflammations, rheumatological pathologies.
- Femoral head necrosis: its causes could be:
- alcoholism
- taking steroids
- unknown origin
What are the major symptoms of the disease?
- Pain that is characterized by the following:
- It presents after waking up in the morning or when remaining in one position for a long time, then it subsides after movement (pain at initiation).
- It increases on loading and during longer walks.
- It eases or resolves at rest.
- In the front of the lower limb, it radiates to the groin, thigh, and towards the knee.
- It is more difficult to extend, abduct, and internally rotate the lower limb in the hip, the hip’s range of motion gradually decreases.
- Reduced ability to walk and reduced walking distance.
- Shortening of the limb.
- All of the above leads to limping.
What are the treatment options?
Non-surgical (conservative) treatment
Aims:
- Reducing the pain
- Increasing the useful range of motion of the joint
- Increasing the muscle strength
- Reducing limping
Methods:
- Pharmacological treatment:
- anti-inflammatory drugs
- painkillers
- antispasmodic drugs, relaxants
- Rheumatological treatment: physiotherapy, medical spa treatment (balneotherapy)
- Exercises aiming for range of motion enhancement
Surgical treatment (operation)
The physician may recommend surgery if the non-surgical treatment methods are ineffective, and the diagnosis is confirmed by clinical examinations and X-ray scans. The timing of the surgery is important, which mostly depends on the patient’s pain tolerance, and the condition of the stabilizing musculature
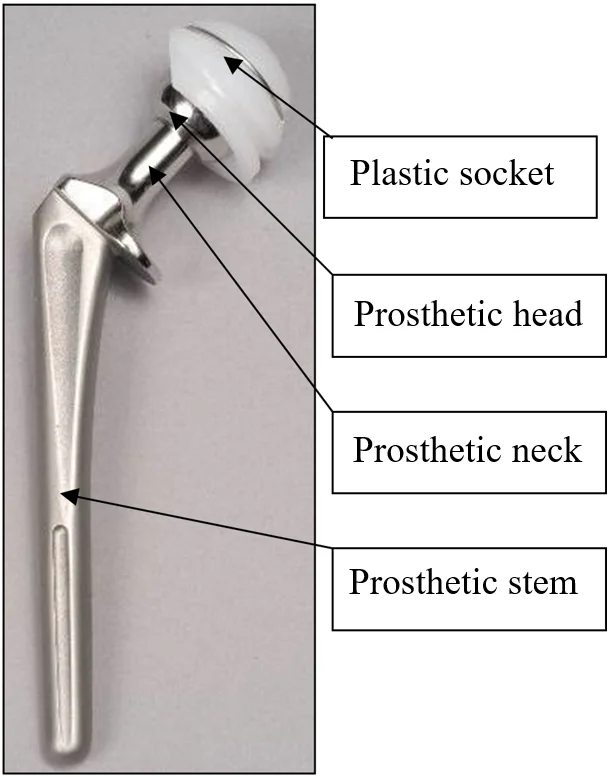
Types of hip prostheses:
- Cemented prosthesis
The socket made out of plastic and the metal stem congruent with the thigh bone are secured to the bone by quickly solidifying adhesive (bone cement).
After the adhesive has solidified, the cemented prosthesis is completely stabile and can bear load. The socket here only consists of the plastic component, which includes a metal ring indicating its location (in the X-ray image). Its disadvantage is that if the implant gets loose, the cement removal is accompanied by bone loss during the prosthesis replacement.
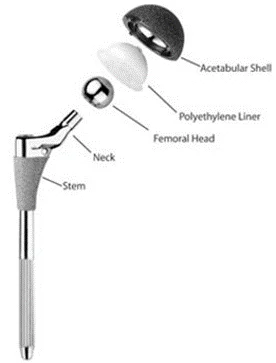
- Uncemented prosthesis
This technique is mostly recommended in young people, and in people below the age of 60 years, when the bone mass is still capable of growing around the prosthetic stem and the socket. No adhesives are used here. In case of an uncemented prosthesis, the socket constitutes of two parts, an external metal cup and a plastic liner. The plastic liner placed in the cup accepts the prosthetic head.
The stem is made of metal (from absolutely tissue-friendly titanium, or titanium coated material), its surface is created in a way to be uneven allowing the bone tissue to fix the implant sufficiently by growing into the uneven spaces. This fixation takes around 2 months, so partial load-relief and complying with gradual loading is necessary (crutches, walking frame).
The life expectancy of cemented as well as uncemented prostheses could be 15-20 years depending on the load, usage, and the condition of the bone mass.
During the surgery, all components of the hip prosthesis are provided from a size series by selecting the optimal size for the patient.
The process of hip endoprosthesis surgery:
- The hip joint could be explored from multiple directions: from the front, the side, and the back.
- Opening the skin and the tissues under the skin is followed by hemostasis (bleeding reduction), then we get to the joint.
- The femoral head is turned out of the socket and the femoral neck is cut with a saw in the correct plane.
- The boney socket is cleared from cartilage and deepened, and the cemented or uncemented artificial socket is placed inside of it.
- This is followed by processing the thigh bone’s medullary cavity.
- The prosthesis is temporarily adjusted in its place, we make sure that the necessary stability is achieved, and the sizes are correct.
- Afterwards, the cemented or uncemented stem component is built in permanently with the artificial joint head.
- The stem is placed into the socket with the head, and a functional test is performed.
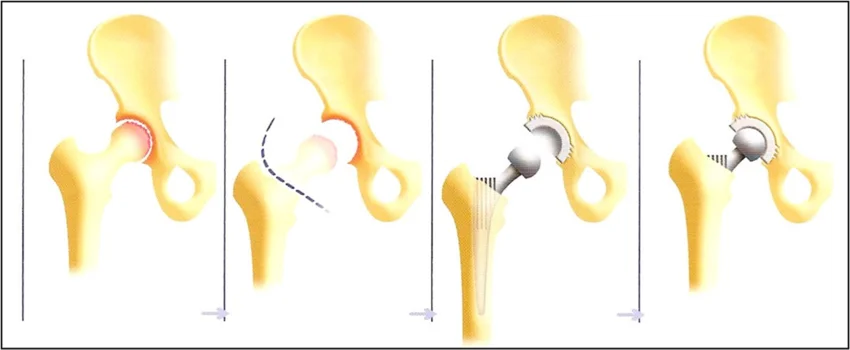
- One or two suction drains are inserted, which will drain the blood accumulating in the wound.
- The wound is sewed (closed), covered with a sterile dressing, and a confirmation X-ray is done while the patient is still on the operating table.
Centrally or individually sterilized instruments, and implants are used for the surgery, which underwent multiple controls.
What happens if the justified surgical treatment is not performed?
- It is expected that the pain increases further.
- The movement disability may aggravate.
- The quality of life will deteriorate further.
- The effectiveness of a later performed surgery may decrease.
If you have any questions, please send a letter to magankorhaz@bhc.hu!







