This is how our application simplifies the booking and administration process. Interested >>
Intervertebral disc herniation surgery
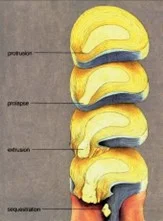
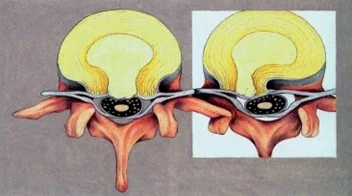
An intervertebral disc herniation means that the concentric rings of the intervertebral disc rupture, and the pulpous material bulges toward the spinal canal causing an hourglass like narrowing. The disease can be treated with non surgical methods, but surgery may be necessary in justified cases.
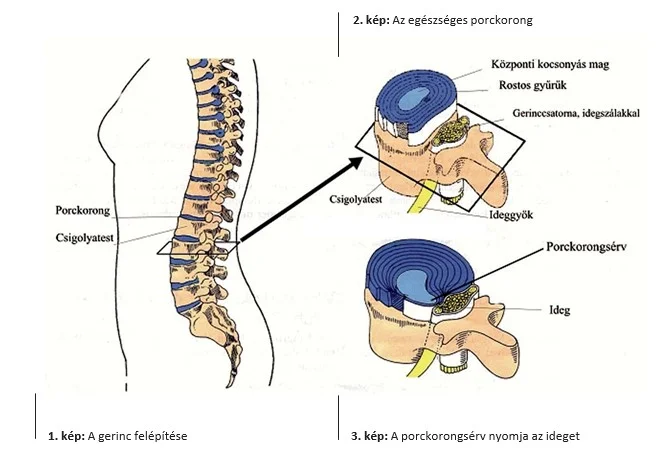
How is a healthy intervertebral disc built?
A healthy intervertebral disc provides a flexible and strong connection between the vertebral bodies. It makes the spine mobile, and it protects it from hits and shakes. It consists of an outer multilayered fibrous wall, and an inner gel like nucleus. The latter is a molecular spatial grid, which physically binds water. The intervertebral disc is a closed space containing water (a hydraulic space), which is nourished through the endplates of the vertebral bodies. Its back wall is richly supplied by sensory nerve endings.
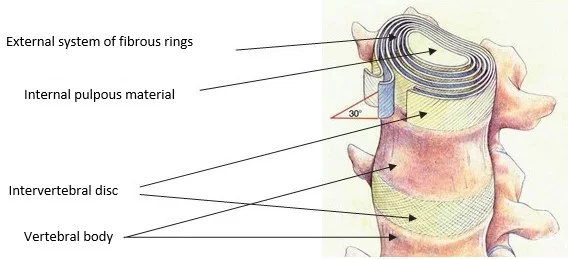
In addition to the intervertebral discs, the vertebrae are linked into a mechanical and biological unit by the strong ligament system, facet joints, and musculature. (These are not shown in Figure 1 for a clearer overview).
What is disc herniation?
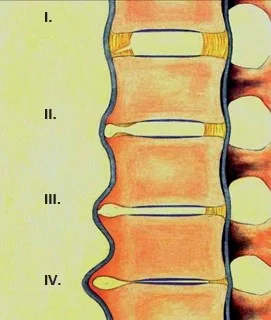
The nucleus of our disc (this is the “perfect gel”) goes through a dehydrating (water loosing) process by the end of our lives’ third decade, which may be significant by the end of the fourth decade. There are discs in the human body, which get injured more frequently, these are the lower discs of the lumbar spine, which are exposed to shear forces in vertical body positions (L4-5 and L5-S1). In addition to aging, genetical differences, injuries, and regular overload may lead to the degeneration of the discs, but this is not necessarily accompanied by herniation.
The fibrous rings, which surround the central pulpous nucleus gradually lose their flexibility, they start to crack and rupture. The central pulpous nucleus may move away from its place, and it pushes the ruptured parts of fibrous ring into the spinal canal. This process is called the herniation of the intervertebral disc.
The bulged disc bit touching the nerve root may first cause the inflammation, then the dysfunction of the nerve. The inflamed nerve gets thicker and even more stuck in the spinal canal, which is narrowed by the herniation.
Which are the potential symptoms of a herniated disc?
- Low back pain, and pain radiating to the lower limb.
- Reduced mobility in the lumbar spine.
- Disturbed sensation or loss of sensation in some areas of the lower limb.
- Weakness, or muscle paralysis of the muscles or muscle groups of the lower limb.
- Pain avoiding, the so called antalgic body posture.
- Vegetative i.e., bowel and urinary incontinence, and sexual dysfunction.
What are the treatment options?
Basically, there are two types of treatment options available:
Non surgical (conservative) treatment
The ruptured bits of the disc may lose the majority of their water content within a few weeks or months, which could make them significantly smaller, or they might even be absorbed. In this case, the nerve compression decreases, and the nerve inflammation abolishes. Oftentimes in a case like that, the symptoms caused by the herniated disc gradually decrease or go away.
Surgical treatment is not used in the first line in those cases, where the nerve is not or only mildly affected, no significant antalgic posture is present, and the pain, which is caused by the herniation, is well tolerated.
The aims of the conservative treatment:
- To reduce nerve inflammation, which leads to
- an increased walking distance,
- reduced pain,
- increased muscle strength.
The methods of conservative treatment:
- Bed rest in the first few days of the treatment (3-4 days).
- Pharmacological and other physiotherapeutic and alternative methods.
The most effective method of conservative treatment is a series of anti inflammatory infusion, and concurrent physiotherapy.
In the long term:
- Lifestyle changes: decreasing/quitting alcohol consumption and smoking, changing the eating habits, decreasing the overweight, decreasing stress, etc.
- Abolishing sleep disturbances, treating the associated psychosomatic diseases (healing the e.g., chronic gynecological, cardiovascular diseases as soon as possible).
- Restoring the mental resilience and the mood.
- Increasing activity: regular physiotherapy, then working out.
Surgery is necessary if improvement is not detected, or if so called neurological (e.g., paralysis) symptoms develop in the lower limb. This way, the nerve can be released from the expressed compression caused by the ruptured herniation.
Surgical treatment of disc herniation
The aim of the surgery is to abolish nerve compression, and the somatic source of the pain. (The surgery does not guarantee that no more herniations will not develop at the same levels of the lumbar spine, or on other intervertebral discs!)
The process of intervertebral disc herniation surgery
- The level of the herniation (segmental level) is marked with an X ray image intensifier.
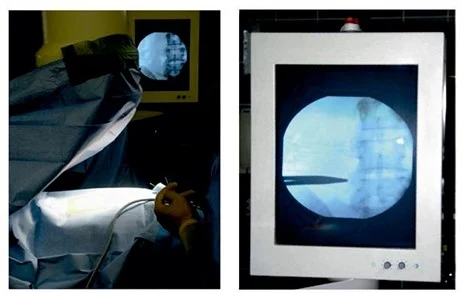
- Usually, a skin incision of 3 5 cm is made on the unhealthy spinal segment.
- Surgical hemostasis is performed after opening the skin and the tissues underneath it.
- The musculature is pushed away from the arches of the adjacent vertebrae, while minding its integrity, then a small opening is created on the back wall of the spine.
- The nerves are held away, then the intervertebral disc herniation is removed with a special instrument.
- In some cases, if it is necessary and anatomically feasible, the defect of the back wall of the intervertebral disc – through which the content of the herniation leaves the volume of the disc – is closed by implanting a tiny implant (the so called “Barricaid®"). This diminishes the risk for a potentially repeated intervertebral disc herniation in the same location.
- A small drain is inserted into the wound, which drains the blood and plasma, which accumulate after the surgery.
- The wound is sewed (closed) in multiple layers, and it is covered with sterile dressing.
What happens if the justified intervertebral disc herniation surgery is not performed?
- The nerve root may get permanently damaged due to the long term compression.
- The pain of the spine and the lower limb may continue to increase.
- The movement disability may aggravate.
- The quality of life may deteriorate further.
- A surgery performed later may become more difficult technically, and its effectiveness may decrease.
What could happen to the movement segment on which surgery was performed due to intervertebral disc herniation?
In the majority of the cases, the resolving limb symptoms allow the physiotherapeutic treatment of the potentially persisting low back pain, the strengthening of the stabilizing musculature, and patients can return to their normal activity. The original state of the operated segment will not be restored, but an acceptable compromise is made, since intervertebral discs might get into a state like that by degeneration and joint wear, even without the development of herniation.
If the adequate stability of the segment is not achieved, – and this does not necessary depend on the time and energy that was put into the exercises and rehabilitation, – increased scarring, and the instability of the segment may develop, and potentially, the herniation may recur. The fixation (stabilization, fusion) of the movement segment with adequate decompression is necessary in a case like that. Very rarely, it is possible to remove the recurred herniation without fixation; this requires individual evaluation, and the symptoms mainly affect the lower limb in these cases.
The process described here can occur at any point in the time scale, but its chance decreases as moving away from the surgery, making the total 5 10%. The adequate healing process can be helped and the above mentioned late consequences can be prevented by taking care, complying with the given advice, loading the spine rationally, and performing not overloading exercises regularly.
If you have any questions, please send a letter to magankorhaz@bhc.hu!