This is how our application simplifies the booking and administration process. Interested >>
Conventional spinal stabilization
Spinal instability may develop due to various causes, and various conservative treatments can be used for it, but in some cases, improvement may only be achieved by surgery. This involves the surgical implantation of metal fixation devices by our physicians, which contribute to the stability of the spine, and the reduction of the symptoms.
The spine protects the spinal cord and the nerves from injuries. The spinal cord is located in the spinal canal, which is bordered by the vertebral bodies and the line of intervertebral discs from the front, and by the vertebral arches and the inbetween ligaments from the back. In addition to its protective function, this structure allows the coordinated movements of the individual spinal levels (movement segments) relative to each other, but it also functions as the inner support of the body. If these functions are compromised, usually in a combined manner, then the movements of the spine become uneven, and instability develops.
As a result of segmental instability, the narrowing of the spinal canal, and the consequential compression of the nerve structures may develop. As protective measures, increased muscle function, and calcified bone spurs (osteophytes) develop later, which try to stabilize the injured joints as a secondary solution.
The causes of spinal instability
- Acute cause
- Injury
- Chronic causes
- Degenerative disease of the spine
- Condition after spine surgery
- Congenital disorder
- Tumor
- Inflammation
The majority of spine diseases are degenerative in nature, which means that they primarily originate from the wear down of the intervertebral discs.
Symptoms of instability:
- Pain, which increases on load:
- Low back pain, pain presenting in a belt like pattern, and pain running down the back outer surface of the lower limb in the direction of the buttocks, thighs, and knees, may originate from the structural components of the spine.
- Pain which radiates below the knees or to the groins and which is accompanied by numbness, pain which is accompanied by numbness and which presents on the front inner surface of the limb may originate from the impingement of nerve structures.
- Limited movements in the spinal segment.
- Disturbed sensation or loss of sensation in some areas of the lower limb.
- Weakness, or muscle paralysis of the muscles or muscle groups of the lower limb.
- Vegetative disorders i.e., bowel or urine incontinence, and sexual dysfunction.
- A pain avoiding, the so called antalgic posture, and limping.
Options:
Conservative (non surgical) treatment
Aims:
- Restoring the stability of the spine, creating a muscle brace.
- Reducing the potential nerve inflammation, which allows:
- The increase of walking distance
- Pain reduction
- The increase of muscle strength
Methods:
- Bed rest in the first few days of the treatment (3 4 days)
- Pharmacological and other physiotherapeutic, and alternative methods
Surgical treatment
The aim of the surgery is to abolish the instability of the spinal segment by implanting a metal fixation device, and to resolve potential nerve compression and the somatic origin of the pain.
The surgical process
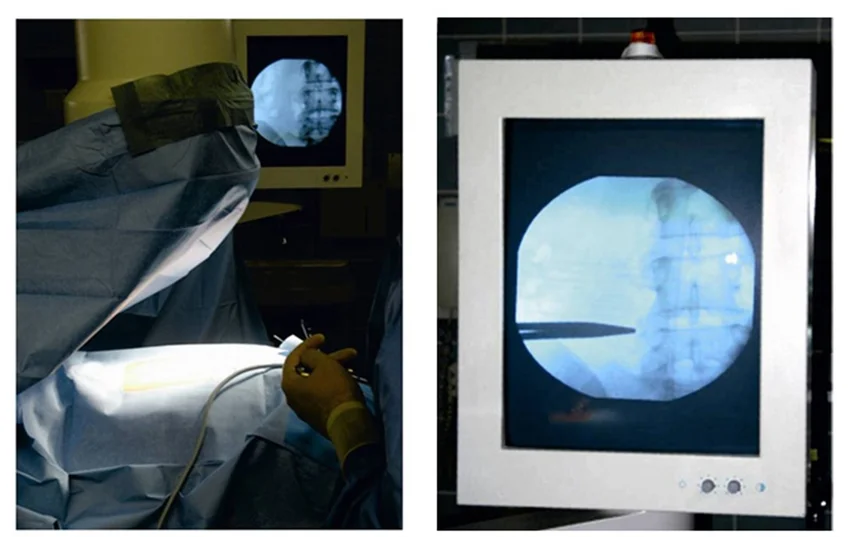
- The level of the narrowing, so the location of the instability is marked by an X ray image intensifier.
- Usually, a skin incision of 12 25 cm is made above the unhealthy spinal segment.
- Surgical hemostasis is performed after opening the skin and the tissues underneath it.
- The musculature is pushed away from the arches of the adjacent vertebrae, while minding its integrity, then a special device is used to remove the necessary soft tissue and bony bits, so that the nerve structures can run freely (decompression).
- The worn down and unusable intervertebral disc is removed, and to maintain the distance between the vertebrae, a spacer is implanted in its place, which is made of titanium or plastic (poly ethyl ethyl carbonate, PEEK) in series sizes, or bone cement that is molded on the spot. In order to achieve bone remodeling later in the affected vertebrae, in addition to the spacer, bone graft material made of the bony bits which were removed from the decompression phase of the surgery, or if necessary, artificial bone substitute is injected in the intervertebral space.
When it comes to stabilization surgeries, the patient’s own bone material is used in most of the cases to fill up the intervertebral spaces, so that bone fusion/bone remodeling will take place with time. The condition for this is that sufficient amount bone tissue (the patient’s own) is available in good quality, which was obtained during the decompression of the nerve structures.
However, there are cases, where neither the quantity, nor the quality of the bone tissue is adequate to achieve bone fusion. In these cases, we have no other choice but to use artificial bone substitutes, or bone material stemming from other humans for our patients. Literature data show that very good results can be achieved by using human bone products in the stimulation of bone remodeling.
The spacer or the bone cement may be injected in the front part of the space (in this case, the bone graft material fills out the area behind the spacer), in the back part, which means that the bone graft material fills the ventral side of the space, or in the complete cavity of the space (in this case, the bone graft material is injected on the vertebral arches). According to our current knowledge, the success of the surgery is not significantly influenced by the relative position of the spacer (cement) and the bone graft material.
What happens if the justified surgery is not performed?
- The nerve root may get permanently damaged due to the long term compression.
- The pain of the spine and the lower limb may continue to increase.
- The movement disability may aggravate.
- The quality of life may deteriorate further.
- A surgery performed later may become more difficult technically, and its effectiveness may decrease.
If you have any questions, please send a letter to magankorhaz@bhc.hu!